Editorial note: The first part of this series was published in issue 1/20 of ceramic implants and can also be found in the News section of this website.
Nowadays, there are still many patients who have lost significant bone volume as a result of tooth extractions and who therefore require bone augmentation measures. In the following second part of the article series “Biological guided bone regeneration and ceramic implants”, six further special techniques are discussed with a focus on the use of autologous materials.
Further special techniques of biological GBR
Dome technique according to Drs Alain Simonpieri and Joseph Choukroun
This technique is used for cases of extremely low residual bone. A collagen sponge flattened to form a membrane is inserted cranially in a folded state, and the cavity is completely filled with PRF membranes. The folded membrane causes a thin bone layer to form a dome-shaped structure between the two membranes in two weeks, generating a stable cavity, necessary for the filling of the lamellar bone. After a healing phase of four to five months, implantation can then take place in a minimally invasive procedure (Figs. 1a–d).
Live donor bone
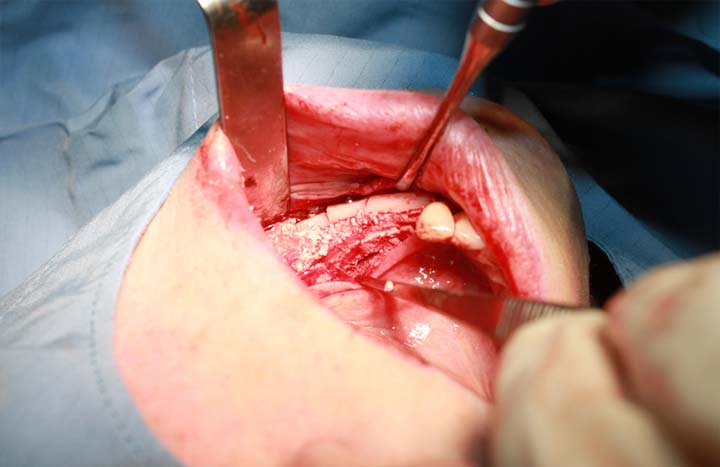
Live donor bone is used when the residual bone height is less than 3 mm or there are large perforations in the alveolar bone (Figs. 2a & b). As this example shows, well-vascularised bone almost completely replaced donor bone after four months (Figs. 3a–g).
Tentpole technique according to Dr Tobias Wilck
A lateral window in the maxillary sinus is fixed with long screws for osteosynthesis and positioned longitudinally in the skull, cranially. In the following example, an umbrella screw was additionally placed according to Dr Markus Schlee (Figs. 4a–e).
Osteosynthesis plate as a temporary placeholder
This technique can only be used in patients without a titanium intolerance. In the case depicted here, this method was used to compensate for the loss of height caused by peri-implantitis (Figs. 5a–d). The volume was constructed in a procedure using an osteosynthesis plate and donor bone, as well as the brushing technique with apical mattress sutures.
The open healing GBR concept according to Prof. Shahram Ghanaati
The research group of Prof. Ghanaati has developed a standardised concept of low-speed centrifugation, which allows reproducible treatment protocols and clinical results. Prof. Ghanaati has managed to show that the composition and bioactivity of PRF depends on the centrifugal force and that a significantly greater number of thrombocytes and leucocytes accumulate at a low centrifugal force, thus releasing higher concentrations of different growth factors.48–50 This extremely interesting, innovative and promising technique elegantly solves the old problem of augmentation coverage with almost complete loss of the keratinised gingiva. The flap is sutured at the basal level and the titanium mesh filled with donor bone is covered only with a collagen membrane and several layers of PRF (low-speed centrifugation) membranes. For initial protection, a sterile latex skin is sutured over the PRF. After healing, the titanium mesh is exposed and can be easily removed. The special feature of this concept is the keratinised gingiva found in the augmented area (Figs. 6a–h).
Khoury layer grafting technique
This technique describes distance osteosynthesis with bone chips (Figs. 7a–d). The extension of the alveolar process/crest of the left mandible was obtained by removing a bone block from the left linea obliqua. The distance screws were inserted for osteosynthesis at a distance, and the defect was filled with bone chips and EthOss (EthOss Regeneration). The defect was covered with PRF membranes, and tight suture closure followed after mobilisation of the mucosa. After three follow-ups, the mucosa was tightly closed. The healing time will be six months in total. We assume that, after the healing phase, well-vascularised bone will be found.
Conclusion
In summary, it can be stated that innumerable biological GBR techniques can be applied. They allow the durable treatment of almost all patient cases. Together with the correct axial positioning of the implant and a prosthetic restoration of lege artis, long-term success depends exclusively on the increased blood supply of the augmented bone (see Mammoto’s law).51 Hence, all of the grafting techniques in this article aim at creating a well-vascularised lamellar de novo bone.
A list of references can be accessed at https://qr.oemus.com/8039
Image credit: Drs Karl Ulrich Volz, Rebekka Hueber, Josephine Tietje, Stephanie Vergote, Tobias Wilck; Prof. Shahram Ghanaati